Continence and Pelvic Health Physiotherapy
Photo: Continence Foundation of Australia
At AMR Physiotherapy, we have two highly experienced Continence and Pelvic Health Physiotherapist’s; Bec Clayton and Lillie Pearse. Bec and Lillie are our specialists in this area, having both completed their Masters in Clinical Physiotherapy (Continence and Women’s Health) at Curtin University in 2017. Bec has been providing Pelvic Health and Women's Health Physiotherapy to the Augusta-Margaret River region for almost 10 years. Learn More
Incontinence (bladder and bowel control problems) and pelvic floor muscle concerns are very common and affect men, women and children. According to the Continence Foundation of Australia, incontinence affects 1 in 4 Australians, prolapse affects up to 50% of women and 1/3 women experience pain during sex (also known as dyspareunia).
The good news is that in many cases these concerns can be improved through lifestyle habits including good bladder and bowel habits, alongside pelvic floor exercises.
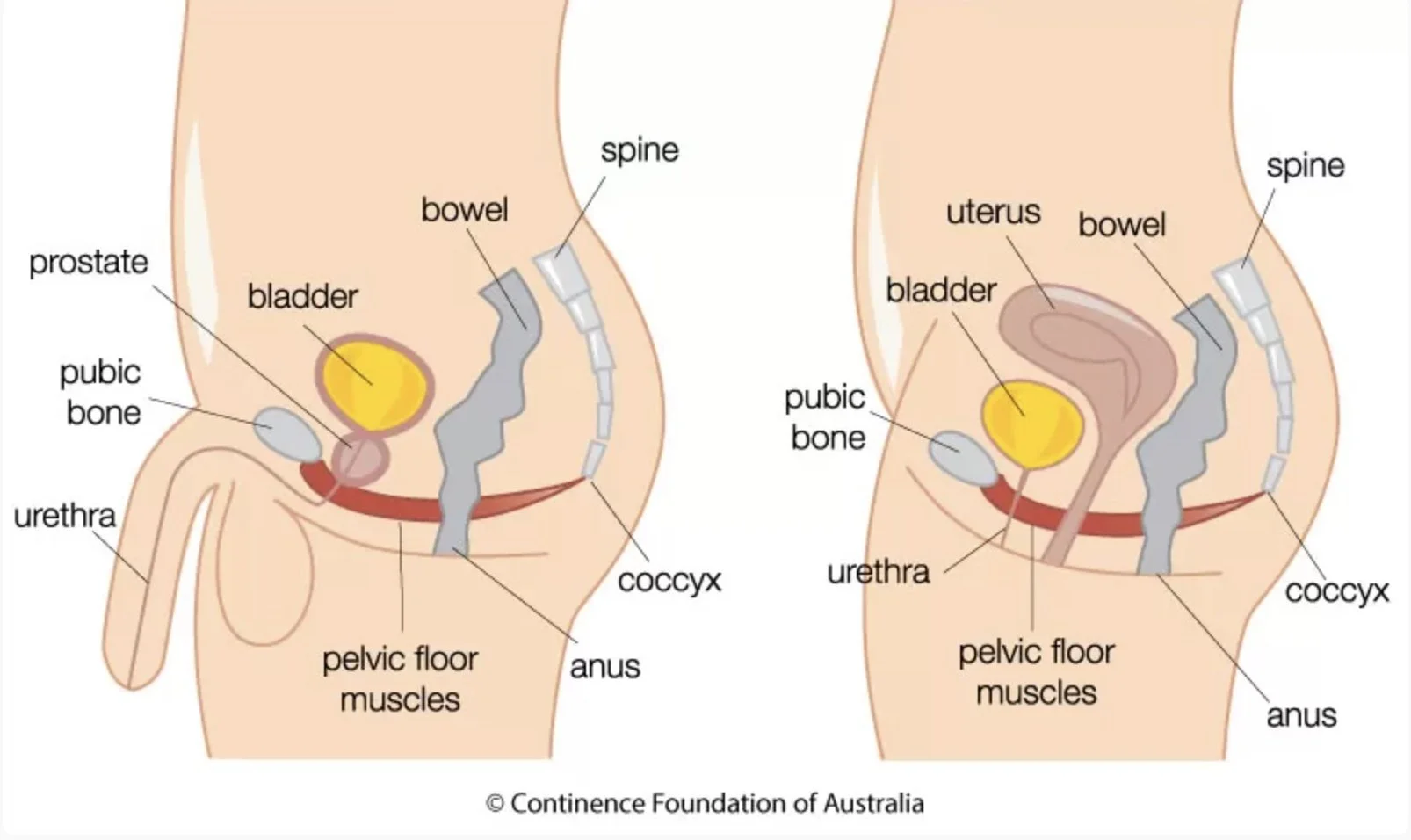
What are the pelvic floor muscles?
The pelvic floor is a hammock of muscles that lie at the bottom of the pelvis. It plays an important role in bladder and bowel control, including being able to empty your bladder and bowel, support of pelvic organs, lower back stability and sexual function. And men have a pelvic floor too! If your pelvic floor muscles are not working properly or effectively, it can result in poor control of the bladder/ bowel and other pelvic floor concerns.
In some people, the pelvic floor muscles have difficulty relaxing, which can cause pelvic floor muscle tightness. A tense pelvic floor may result in difficulty emptying the bladder or bowel, pelvic pain or pain during sex.
Symptoms of pelvic floor muscle concerns
Bladder and bowel control problems such as incontinence
Pelvic organ prolapse
Overactive bladder
Constantly needing to empty your bladder or difficulty emptying your bladder
Feeling an urgent need to empty your bladder or bowel (urgency)
Constipation, difficulty emptying your bowel
Pelvic pain such as endometriosis
Vaginal or vulval pain (vulvodynia)
Pain during sexual intercourse (dyspareunia, vaginismus)
What can be done to improve incontinence and pelvic floor muscle concerns?
Supervised pelvic floor muscle exercises are recommended as the first line of treatment for men and women with urinary incontinence (International Continence Society 2013)
Pelvic floor muscle exercises can improve prolapse symptoms and severity (International Continence Society 2013)
It is not as simple as squeezing and lifting… most people try too hard!
Many people have difficulty isolating the pelvic floor muscles and approximately half of women who learn pelvic floor muscle exercises from a brochure perform the wrong technique (Continence Foundation of Australia). Performing the wrong technique may actually make your problem worse.
We also treat
Pregnant/ antenatal or postnatal women with neck, back, pelvic, coccyx or wrist pain
Antenatal women for education, preparation for birth and exercise prescription
Postnatal women for
Painful episiotomy or perineal tears- we have a therapeutic ultrasound machine which can help with perineal pain including haemorrhoids following birth
Weak or separated abdominal muscles
Blocked ducts & mastitis- we have a therapeutic ultrasound machine which can help with blocked ducts or mastitis
Bladder/ bowel dysfunction
Return to exercise including running
Men health- for example men who have pelvic floor concerns or who have undergone prostate cancer treatment
Women who are having or have undergone gynaecological or urological surgery
Peri or postmenopausal women with pelvic floor muscle dysfunction
Bec and Lillie will thoroughly assess your problem, explain your condition, customize an individualized exercise program to suit your needs and ensure you are performing the correct technique. They have a real-time ultrasound machine which provides an image of the pelvic floor in action, giving you instant feedback to help you learn the correct pelvic floor muscle contraction.
Initial appointments are one hour, to allow time to thoroughly understand and assess your problem. Subsequent appointments are 45 minutes in length. Assessment and treatment are carried out in a private, sensitive environment as we understand that it can be difficult to talk about these problems.
If you experience any of the above problems or are unsure if you should seek help please contact us
You do not require a GP/ doctor’s referral to see Bec or Lillie.